PROTON THERAPY FOR BRAIN AND SPINE TUMORS
Proton therapy is the latest and advanced form of radiation treatment that uses a beam of protons to deliver radiation precisely and effectively to Tumors while sparring normal tissues .
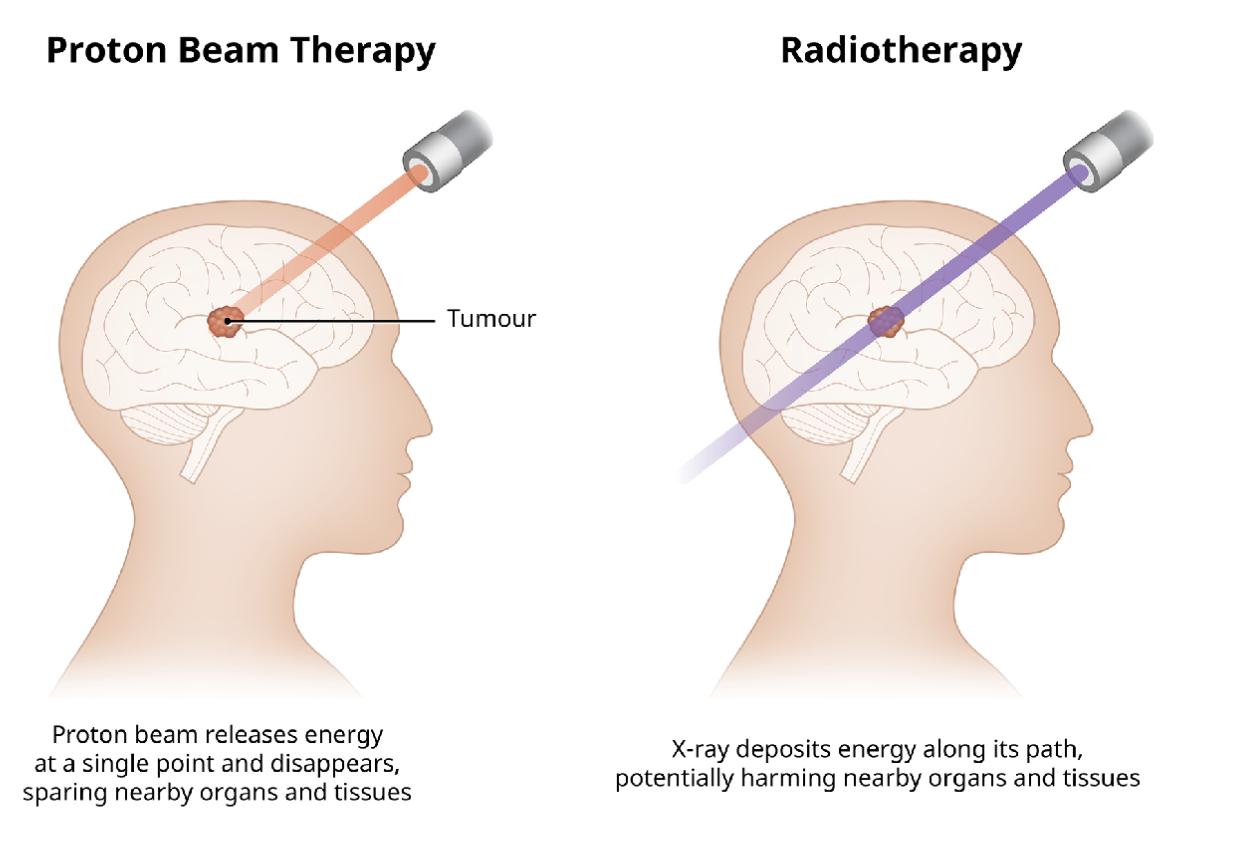
Proton therapy is a type of radiation therapy that uses a beam of protons to treat cancer and some noncancerous tumors. Protons are positively charged particles that can damage the DNA of cells and stop their reproduction, thus killing them. Proton therapy has some advantages over current types of radiation therapy, such as X-rays, because protons can be more precisely controlled to target the tumor and spare the surrounding healthy tissue. Proton therapy may cause fewer side effects than traditional radiation. It is not widely available except in advanced overseas centers such as MD Anderson Cancer center in Texas, USA states Dr Prem Pillay, a Singapore Neurosurgeon who was a Fellow in Neurosurgical Oncology (Brain and Spine Tumors) at MD Anderson Cancer Center and is now practising at the Singapore Brain-Spine-Nerves Center at the Mt Elizabeth Medical Center in Singapore. Fortunately for patients in our part of Asia, Proton therapy is now available at Mt Elizabeth Hospitals, in Singapore.
Proton therapy is performed using a particle accelerator that produces a beam of protons. The beam is shaped and directed by magnets and computers to match the size and shape of the tumor. The patient lies on a table that can be moved and rotated to adjust the position of the beam. The treatment usually lasts for several minutes and may be given in small doses (fractionation) daily for a few weeks to improve results and reduce side effects.
What tumors can Proton Therapy Treat?
Proton therapy may be used to treat various types of brain, spine, breast, eye, esophageal, head and neck, liver, lung, lymphoma, pancreatic, prostate, sarcoma, chordomas, gliomas. It may also be used to treat children, who are more sensitive to radiation damage. Proton therapy may be used alone or in combination with other treatments, such as surgery and chemotherapy. Proton therapy may also be used if tumor remains or comes back after traditional X-ray radiation. Brain tumors that can be treated include Malignant Gliomas such as Glioblastomas, Astrocytomas, Ependymomas,aggressive pituitary tumors, Meningiomas, Brain cancer/metastases that has spread to the brain from the breast , lung, and other primary sites.Skull base tumors such as Chordoma, Chondrosarcoma, adenocarcinoma, squamous cell carcinoma to name a few are can also be potentially treated with proton therapy. Spine tumors and cancer can also be treated. Proton therapy can target t tumors with a sub-millimeter precision while sparring nearby healthy tissues and minimizing side effects.
Standard radiation therapy has evolved and improved over the years and is effective in controlling many cancers. However, because X-ray beams are composed of primary photons and secondary electrons, they deposit their energy along the path of the beam, to the targeted tumor and beyond, and deliver radiation to healthy tissues before and after the tumor site. This radiation “exit dose” may cause health issues later because it can damage the normal tissue or organs near the tumor or area of concern.
The advantage of proton therapy (also called proton beam therapy) is that the physician can control where the proton releases the bulk of its cancer-fighting energy. As the protons move through the body, they slow down and interact with electrons, and release energy. The point where the highest energy release occurs is the “Bragg peak.” A physician can designate the Bragg peak’s location, causing the most damage to the targeted tumor cells. A proton beam conforms to the shape and depth of a tumor while sparing healthy tissues and organs.
How Dose Proton Therapy actually work?
The best way to understand how proton therapy works is to take a look at the physics and engineering inside the proton accelerator, or the synchrotron, and the beam delivery system.
The proton begins its journey at the ion source. Within fractions of a second, hydrogen atoms are separated into negatively charged electrons and positively charged protons.
The protons are injected via a vacuum tube into a linear accelerator and in only a few microseconds, the protons’ energy reaches 7 million electron volts.
Proton beams stay in the vacuum tube as they enter the synchrotron, where acceleration increases their energy to a total of 70 million to 250 million electron volts, enough to place them at any depth within the patient’s body.
After leaving the synchrotron, the protons move through a beam-transport system comprised of a series of magnets that shape, focus and direct the proton beam to the appropriate treatment room.
To ensure that each patient receives the prescribed treatment safely and efficiently, the facility is controlled by a network of computers and safety systems. The gantry can revolve around the patient, allowing the beam to be delivered through many angles.
As protons come through the nozzle, a custom-made device (the aperture) shapes the beam of protons, and another custom-made device (the compensator) shapes the protons into three dimensions, delivering them to the depth of the tumor.
At maximum energy, a proton beam travels 125,000 miles per second, which is equivalent to the two-thirds the speed of light.
Pencil beam and intensity modulated proton therapy
The team at MD Anderson Proton Therapy Center has continued to expand ways to use proton therapy to benefit patients. The team pioneered pencil beam proton therapy, also called scanning beam, and intensity modulated proton therapy (IMPT). The techniques are now available to other treatment centers said Dr Prem Pillay.
Pencil beam technology and IMPT build on the benefits of proton therapy. With a proton beam just millimeters wide, these advanced forms of proton therapy combine precision and effectiveness, offering unmatched ability to treat a patient’s tumor and minimizing the effect on a patient’s quality of life – during and after treatment. They rely on complex treatment planning systems and an intricate number of magnets to aim a narrow proton beam and essentially “paint” a radiation dose layer by layer.
Pencil beam is very effective in treating the most complex tumors, like those in the Brain, Spine,eye, and cancers in children, while leaving healthy tissue and other critical areas unharmed. IMPT is best used to deliver a potent and precise dose of protons to complex or concave-shaped tumors that may be adjacent to the spinal cord or embedded head and neck or skull base below the brain or around brain critical structures.
For more information on Proton Therapy for Brain and Spine tumors kindly contact us at +6568354325.
References:
1.Towards effective and efficient patient-specific quality assurance for spot scanning proton therapy
X Ronald Zhu 1 , Yupeng Li 2 , Dennis Mackin 3 , Heng Li 4 , Falk Poenisch 5 , Andrew K Lee 6 , Anita Mahajan 7 , Steven J Frank 8 , Michael T Gillin 9 , Narayan Sahoo 10 , Xiaodong Zhang 11
Cancers (Basel) 2015 Apr 10;7(2):631-47.
Affiliations : MD Anderson Cancer Center
2.Proton Therapy for Head and Neck Cancer: A 12-Year, Single-Institution Experience
G Brandon Gunn 1 , Adam S Garden 1 , Rong Ye 2 , Noveen Ausat 1 , Kristina R Dahlstrom 3 , William H Morrison 1 , C David Fuller 1 , Jack Phan 1 , Jay P Reddy 1 , Shalin J Shah 1 , Lauren L Mayo 1 , Stephen G Chun 1 , Gregory M Chronowski 1 , Amy C Moreno 1 , Jeffery N Myers 3 , Ehab Y Hanna 3 , Bita Esmaeli 4 , Maura L Gillison 5 , Renata Ferrarotto 5 , Katherine A Hutcheson 3 , Mark S Chambers 3 , Lawrence E Ginsberg 6 , Adel K El-Naggar 7 , David I Rosenthal 1 , Xiaorong Ronald Zhu 8 , Steven J Frank 1
Int J Part Ther. 2021 Jun 25;8(1):108-118.