PARKINSON’S DISEASE

Parkinson’s disease is a brain disorder that leads to shaking, stiffness, and difficulty with walking, balance, and coordination.
Parkinson’s symptoms usually begin gradually and get worse over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.
Both men and women can have Parkinson’s disease. However, the disease affects about 50 percent more men than women.
One clear risk factor for Parkinson’s is age. Although most people with Parkinson’s first develop the disease at about age 60, about 5 to 10 percent of people with Parkinson’s have “early-onset” disease, which begins before the age of 50. Early-onset forms of Parkinson’s are often, but not always, inherited, and some forms have been linked to specific gene mutations.
What Causes Parkinson’s Disease?
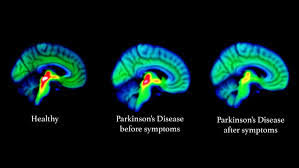
Parkinson’s disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinson’s. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many automatic functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinson’s contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinson’s disease and Lewy body dementia.
Although some cases of Parkinson’s appear to be hereditary, and a few can be traced to specific genetic mutations, in most cases the disease occurs randomly and does not seem to run in families. Many researchers now believe that Parkinson’s disease results from a combination of genetic factors and environmental factors such as exposure to toxins.
Symptoms of Parkinson’s Disease
Parkinson’s disease has four main symptoms:
- Tremor (trembling) in hands, arms, legs, jaw, or head
- Stiffness of the limbs and trunk
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include depression and other emotional changes; difficulty swallowing, chewing, and speaking; urinary problems or constipation; skin problems; and sleep disruptions.
Symptoms of Parkinson’s and the rate of progression differ among individuals. Sometimes people dismiss early symptoms of Parkinson’s as the effects of normal aging. In most cases, there are no medical tests to definitively detect the disease, so it can be difficult to diagnose accurately.
Early symptoms of Parkinson’s disease are subtle and occur gradually. For example, affected people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinson’s. They may see that the person’s face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s often develop a parkinsonian gait that includes a tendency to lean forward, small quick steps as if hurrying forward, and reduced swinging of the arms. They also may have trouble initiating or continuing movement.
Symptoms often begin on one side of the body or even in one limb on one side of the body. As the disease progresses, it eventually affects both sides. However, the symptoms may still be more severe on one side than on the other.
Many people with Parkinson’s note that prior to experiencing stiffness and tremor, they had sleep problems, constipation, decreased ability to smell, and restless legs.
Diagnosis of Parkinson’s Disease
A number of disorders can cause symptoms similar to those of Parkinson’s disease. People with Parkinson’s-like symptoms that result from other causes are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinson’s, certain medical tests, as well as response to drug treatment, may help to distinguish them from Parkinson’s. Since many other diseases have similar features but require different treatments, it is important to make an exact diagnosis as soon as possible.
There are currently no blood or laboratory tests to diagnose nongenetic cases of Parkinson’s disease. Diagnosis is based on a person’s medical history and a neurological examination. Improvement after initiating medication is another important hallmark of Parkinson’s disease.
Treatment of Parkinson’s Disease
Although there is no cure for Parkinson’s disease, medicines, surgical treatment, and other therapies can often relieve some symptoms.
Medicines for Parkinson’s Disease
- Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy—such as nausea, vomiting, low blood pressure, and restlessness—and reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinson’s symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Deep Brain Stimulation
For people with Parkinson’s who do not respond well to medications, deep brain stimulation, or DBS, may be appropriate. DBS is a surgical procedure that surgically implants electrodes into part of the brain and connects them to a small electrical device implanted in the chest. The device and electrodes painlessly stimulate the brain in a way that helps stop many of the movement-related symptoms of Parkinson’s, such as tremor, slowness of movement, and rigidity. This is now an established method to treat patients with the disease who are not responding to medications and are progressing explained Dr Prem Pillay a Singapore Neurosurgeon who trained at the Cleveland Clinic-USA and is now Medical Director at the Singapore Brain Spine Nerves Center.
Other Therapies
Other therapies may be used to help with Parkinson’s disease symptoms. They include physical, occupational, and speech therapies, which help with gait and voice disorders, tremors and rigidity, and decline in mental functions.
Neuropsychological assessment and support is useful. Aquatic physiotherapy is also a useful treatment to improve Parkinsons Disease.
Table Tennis for Parkinsons Disease is another exercise that is beneficial for muscle coordination and balance.
Other supportive therapies include a healthy diet and adequate quality sleep.
References and Acknowledgements
National Institutes of Health-USA
Singapore Brain Spine Nerves Center
Table Tennis for Good Foundation
