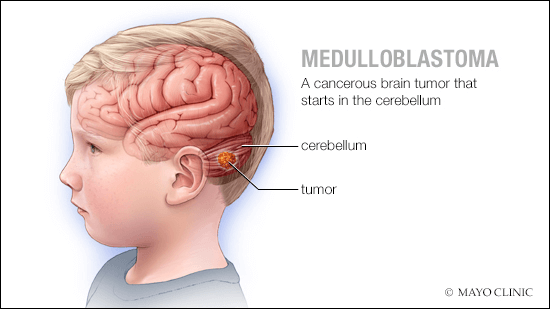
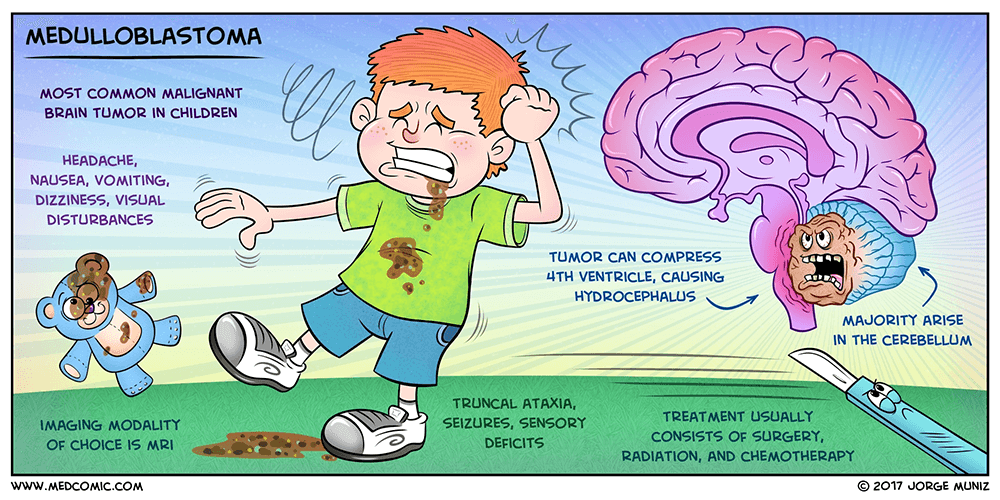
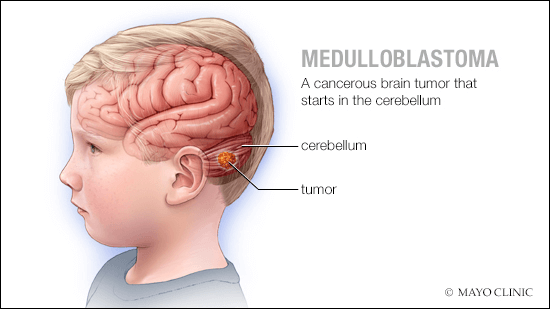
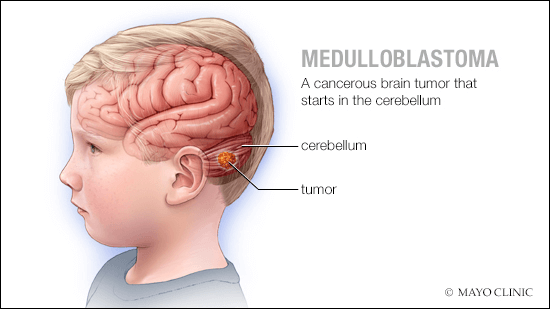
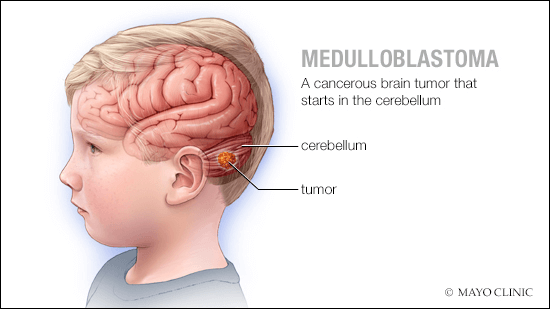
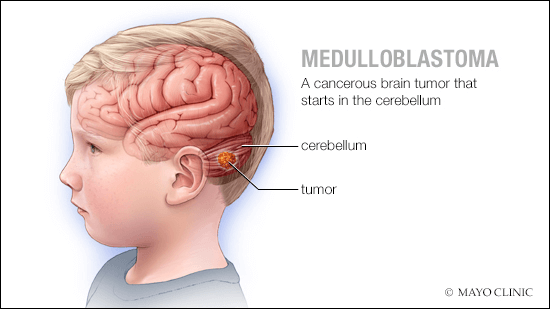
MEDULLOBLASTOMA
Definition
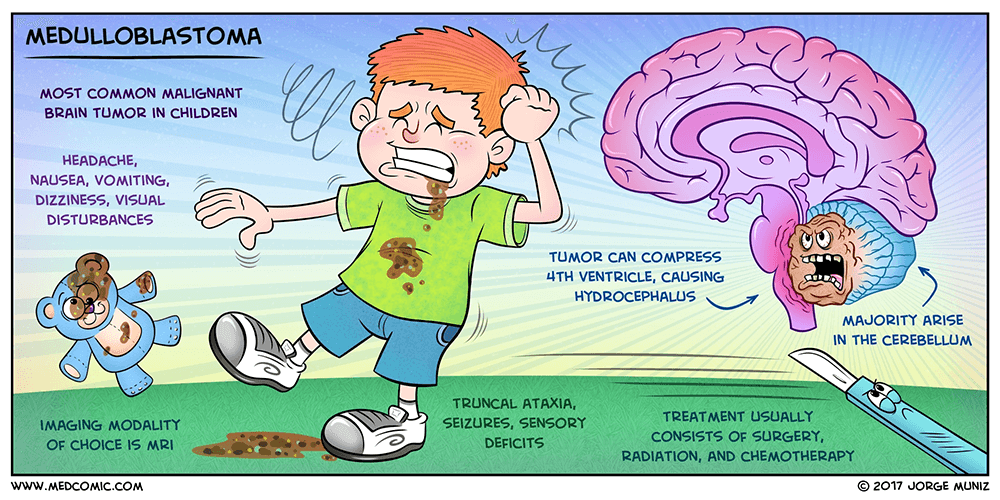
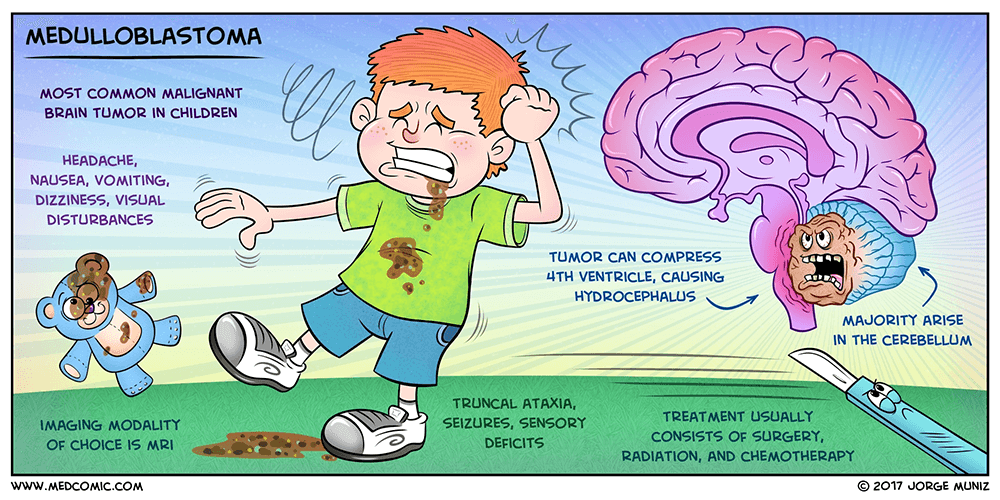
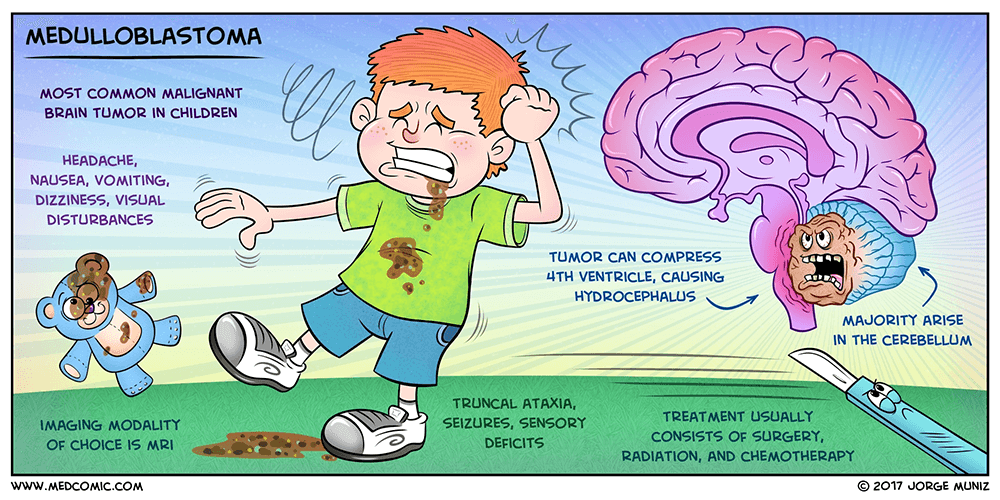
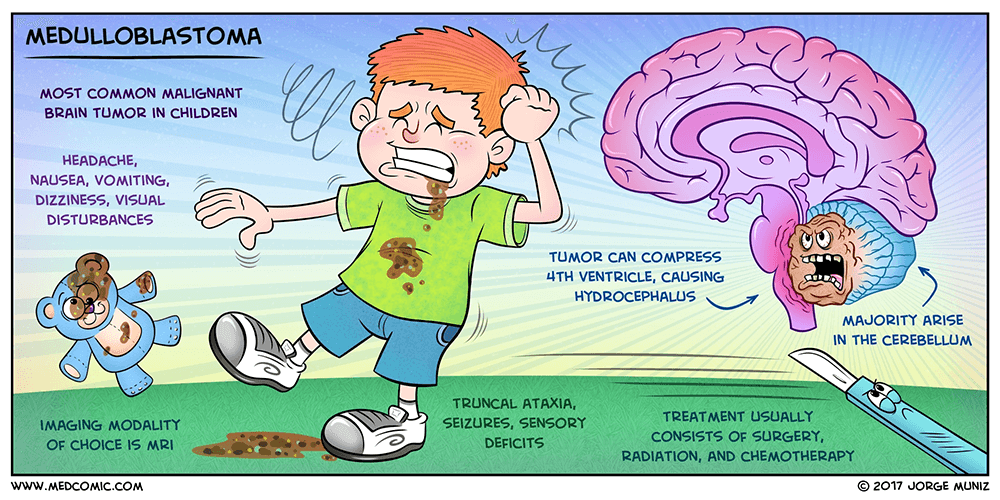
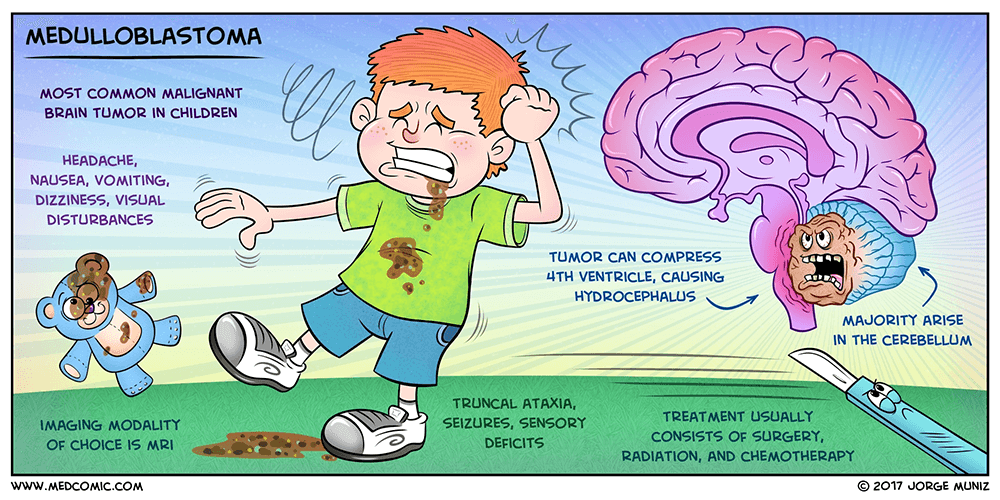
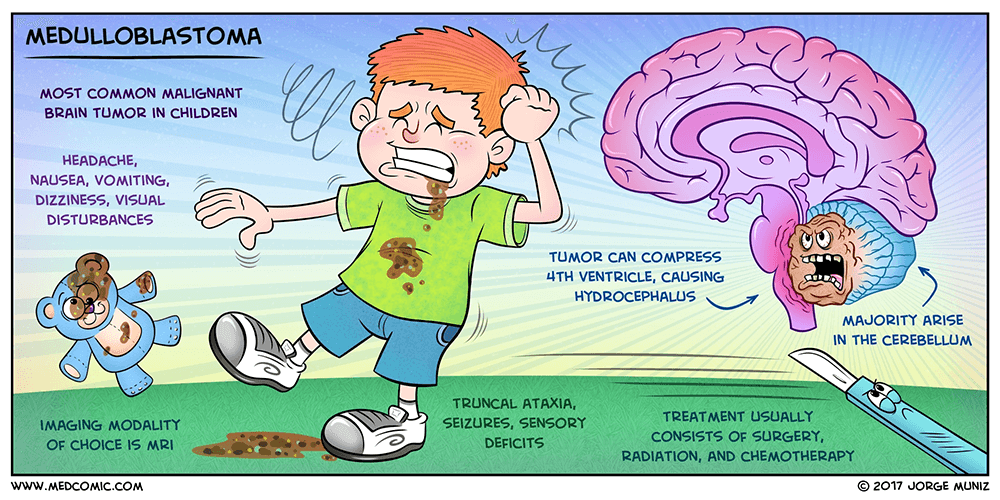
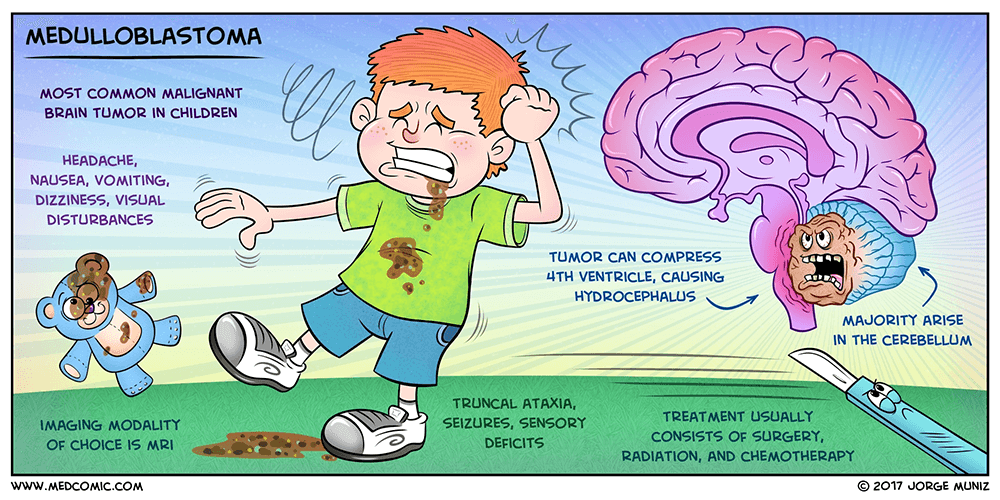
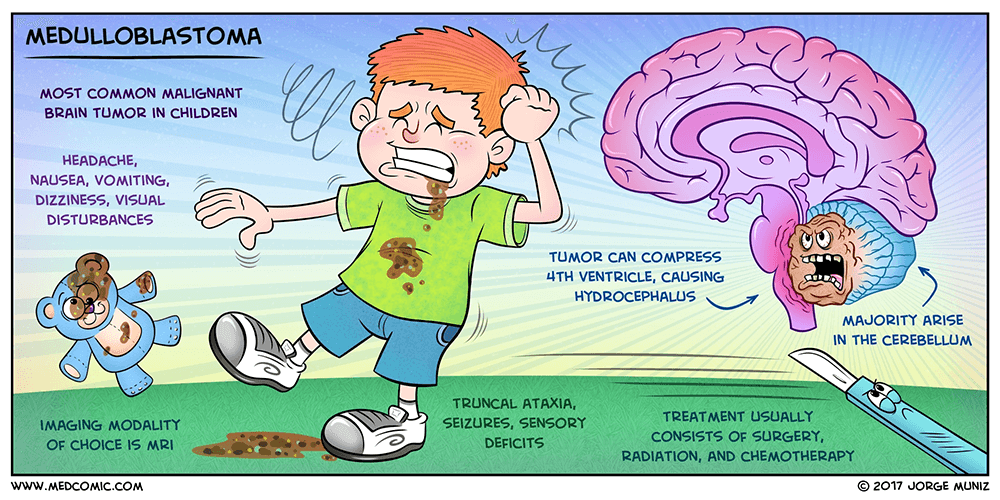
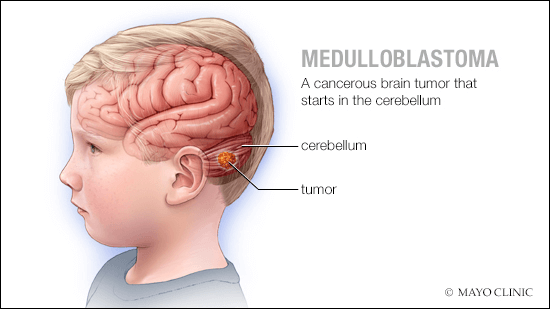
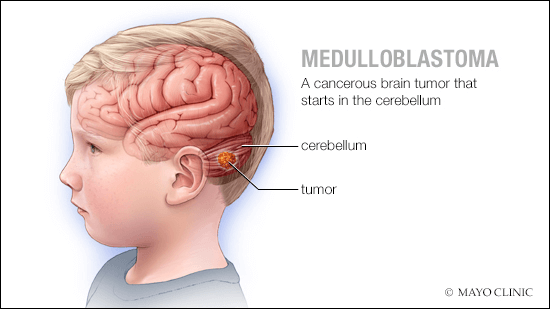
Medulloblastoma (MB) is an embryonic tumor of the neuroepithelial tissue and the most frequent primary pediatric solid malignancy. MB represents a heterogeneous group of cerebellar tumors characterized clinically by increased intracranial pressure and cerebellar dysfunction, with the most common presenting symptoms being headache, vomiting, and ataxia.
Epidemiology
MB is the most common malignant brain tumor in childhood. Annual incidence is estimated at 1/909,000 in Europe, 1.5/100,00 in the USA said Dr Prem Pillay , a Neurosurgeon who specializes in treating Medulloblastomas ( He trained at the Cleveland Clinic,USA and the Hospital for Sick Children, Toronto. Males are more affected than females.
Clinical description
Etiology
To date, the exact etiology of MB is still unknown but genomic data has identified multiple candidate genes that contribute to the pathogenesis of different subgroups of MB. This includes an inhibitor of the sonic hedgehog pathway SUFU (10q24.32), the RNA helicase DDX3X (Xp11.3-p11.23), chromatin regulators KDM6A (Xp11.2) and N-CoR complex genes BCOR (Xp11.4), and the Parkinson’s disease genes KMT2D (12q13.12), SMARCA4 (19p13.3), MYCN (2p24.3), and TP53 (17p13.1).
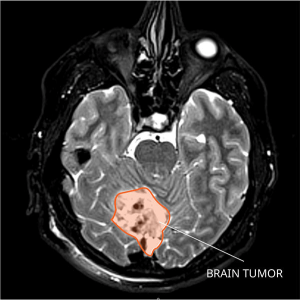
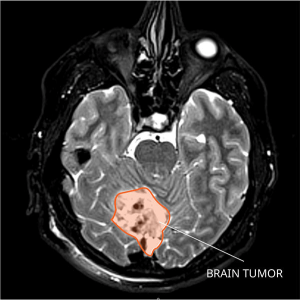
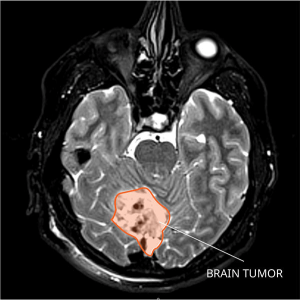
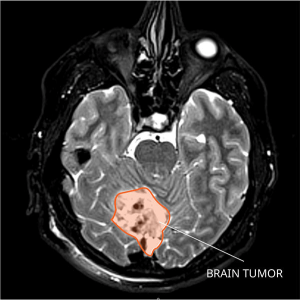
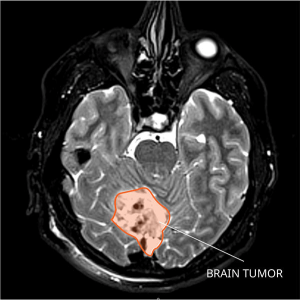
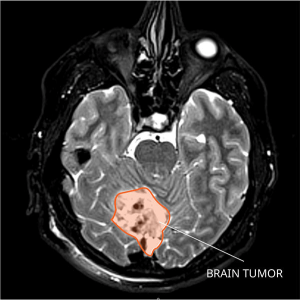
Diagnostic methods





Differential diagnosis
Differential diagnosis includes other brain tumors (ependymoma, glial tumor, atypical teratoid rhabdoid tumor; see these terms) and other causes of cerebellar alterations (infectious or cystic lesions, hemorrhages).
Management and treatment
Initially, patients need to be checked for increased intracranial pressure, which if present, needs to be controlled either by drugs (e.g. steroids) or by neurosurgical drainage (e.g. external drainage).
The best current treatment is gross total resection of the Tumor using Microsurgery assisted with Computer aided Image guided technology, Neuromonitoring particularly of brainstem signals followed by good ICU care stated Dr Prem Pillay who specializes in brain tumors including Medulloblastomas. The postoperative treatment depends on age, histological variant, and result of staging assessments. In children older than 3-5 years, combinations of chemotherapy and craniospinal irradiation including Stereotactic Radiotherapy with MicroMLC technology can be applied. In younger children, brain sparing therapies avoiding irradiation can be administered in very specific constellations.
Prognosis
The overall survival rates are now 80% in standard risk patients, and 30-60 % in high-risk patients.
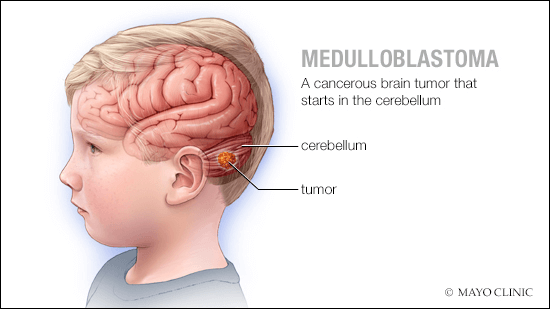
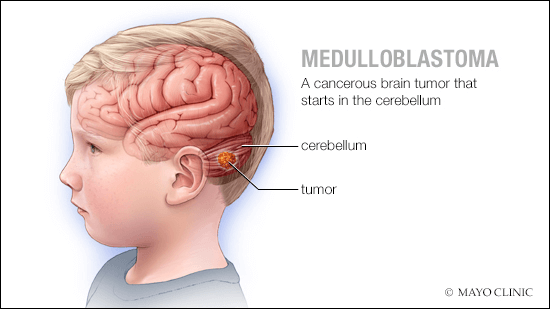
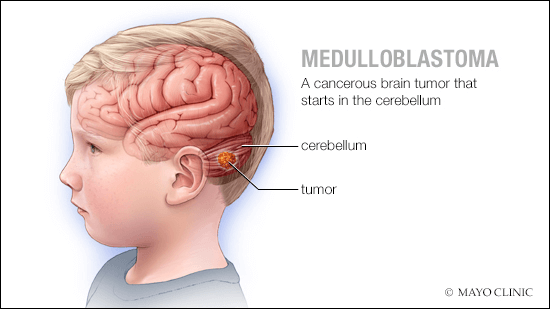
MEDULLOBLASTOMA
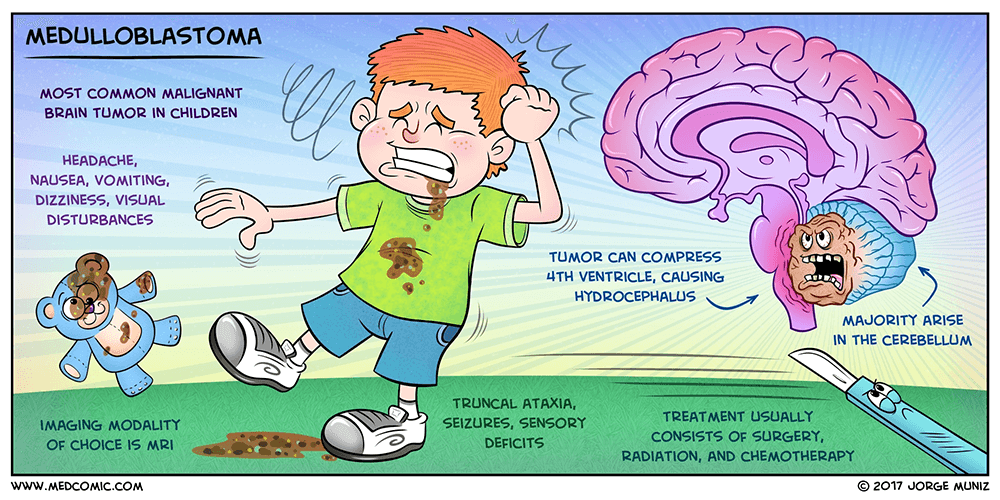
Definition
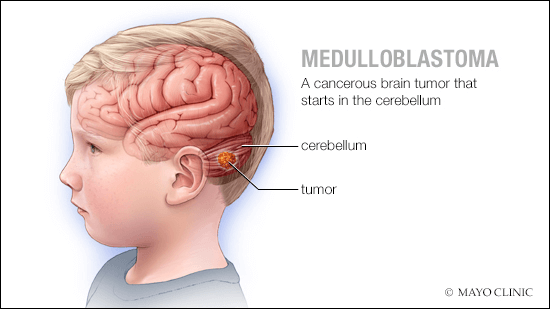
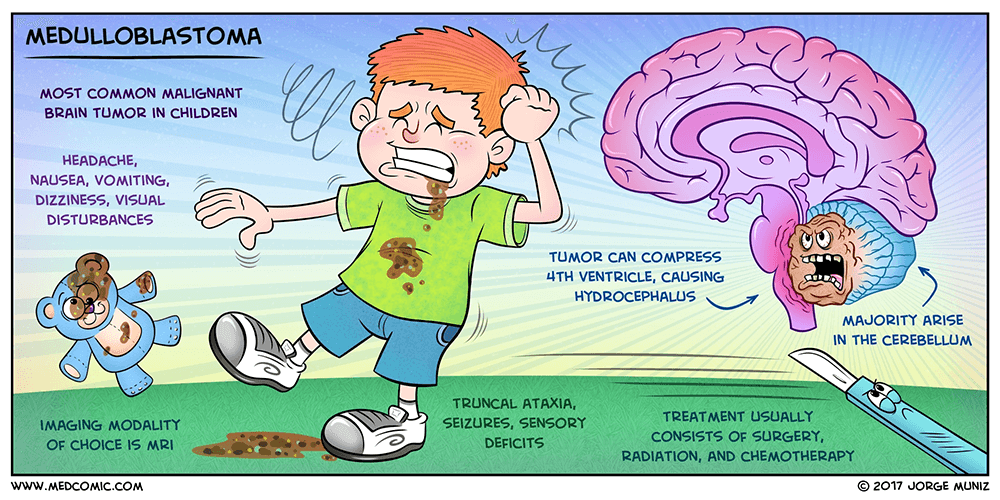
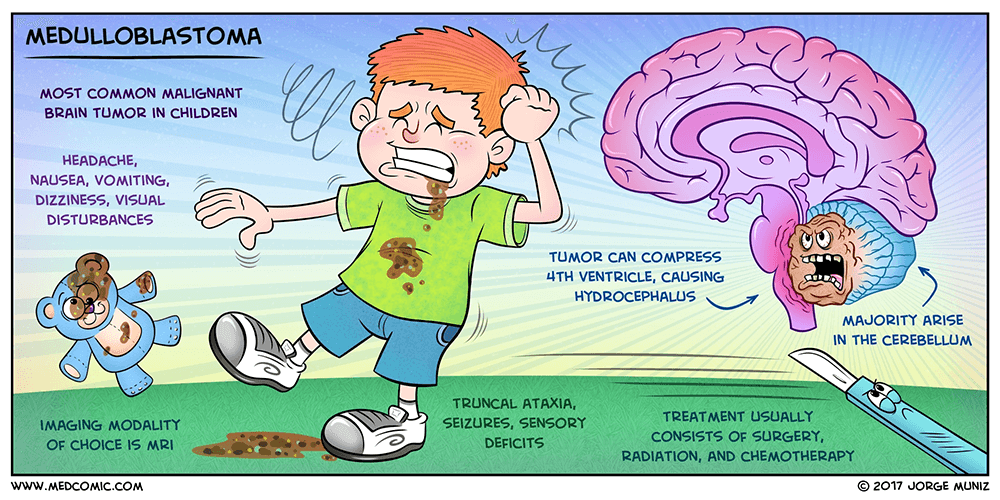
Medulloblastoma (MB) is an embryonic tumor of the neuroepithelial tissue and the most frequent primary pediatric solid malignancy. MB represents a heterogeneous group of cerebellar tumors characterized clinically by increased intracranial pressure and cerebellar dysfunction, with the most common presenting symptoms being headache, vomiting, and ataxia.
Epidemiology
MB is the most common malignant brain tumor in childhood. Annual incidence is estimated at 1/909,000 in Europe, 1.5/100,00 in the USA said Dr Prem Pillay , a Neurosurgeon who specializes in treating Medulloblastomas ( He trained at the Cleveland Clinic,USA and the Hospital for Sick Children, Toronto. Males are more affected than females.
Clinical description
Etiology
To date, the exact etiology of MB is still unknown but genomic data has identified multiple candidate genes that contribute to the pathogenesis of different subgroups of MB. This includes an inhibitor of the sonic hedgehog pathway SUFU (10q24.32), the RNA helicase DDX3X (Xp11.3-p11.23), chromatin regulators KDM6A (Xp11.2) and N-CoR complex genes BCOR (Xp11.4), and the Parkinson’s disease genes KMT2D (12q13.12), SMARCA4 (19p13.3), MYCN (2p24.3), and TP53 (17p13.1).
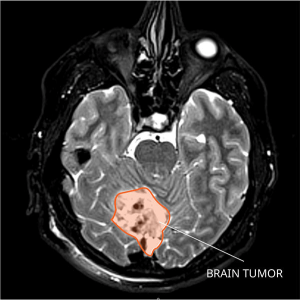
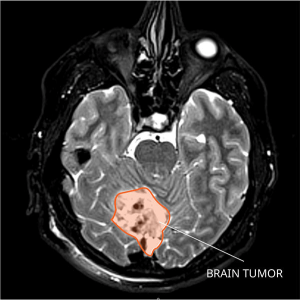
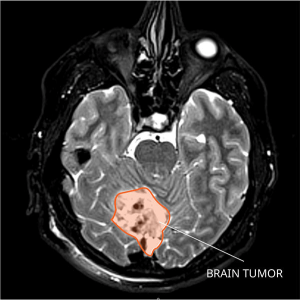
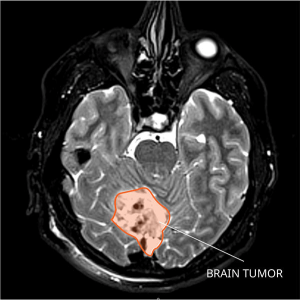
Diagnostic methods





Differential diagnosis
Differential diagnosis includes other brain tumors (ependymoma, glial tumor, atypical teratoid rhabdoid tumor; see these terms) and other causes of cerebellar alterations (infectious or cystic lesions, hemorrhages).
Management and treatment
Initially, patients need to be checked for increased intracranial pressure, which if present, needs to be controlled either by drugs (e.g. steroids) or by neurosurgical drainage (e.g. external drainage).
The best current treatment is gross total resection of the Tumor using Microsurgery assisted with Computer aided Image guided technology, Neuromonitoring particularly of brainstem signals followed by good ICU care stated Dr Prem Pillay who specializes in brain tumors including Medulloblastomas. The postoperative treatment depends on age, histological variant, and result of staging assessments. In children older than 3-5 years, combinations of chemotherapy and craniospinal irradiation including Stereotactic Radiotherapy with MicroMLC technology can be applied. In younger children, brain sparing therapies avoiding irradiation can be administered in very specific constellations.
Prognosis
The overall survival rates are now 80% in standard risk patients, and 30-60 % in high-risk patients.
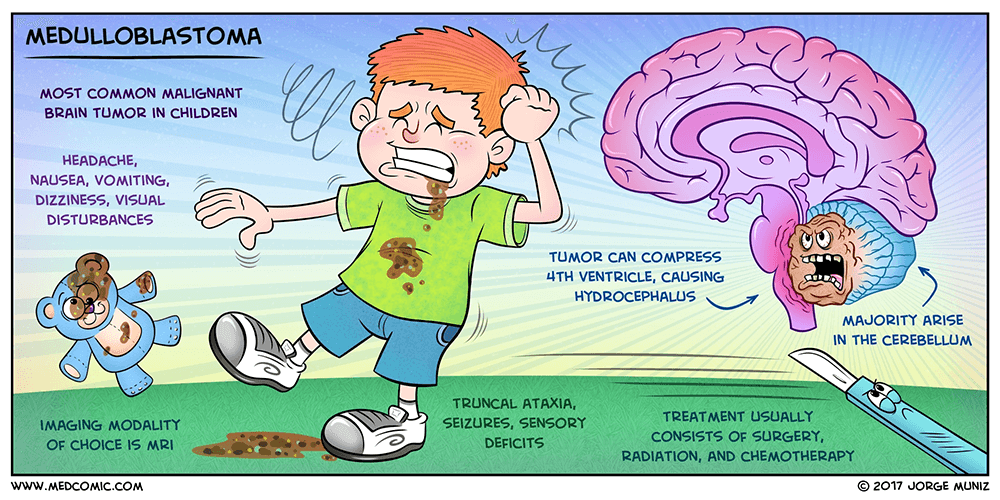
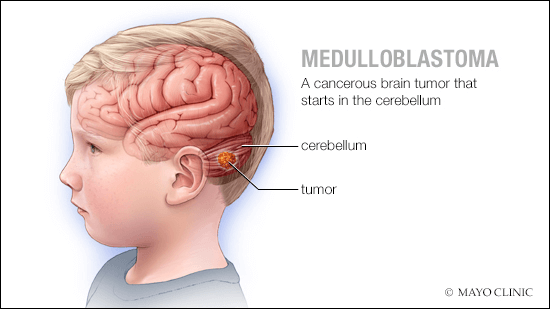
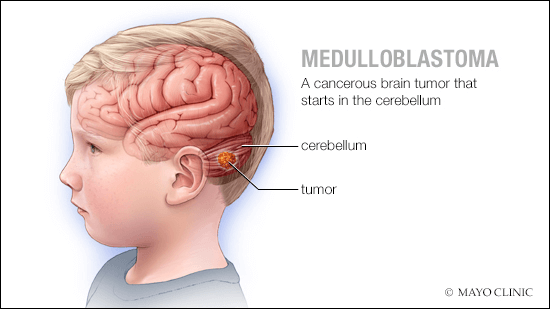
MEDULLOBLASTOMA
Definition
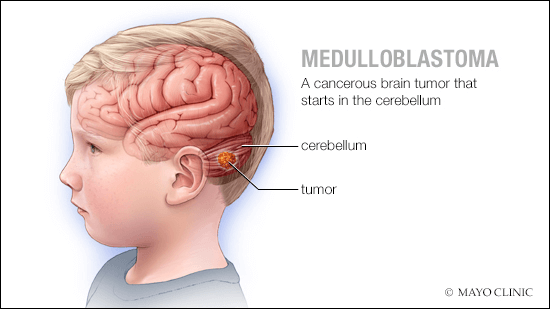
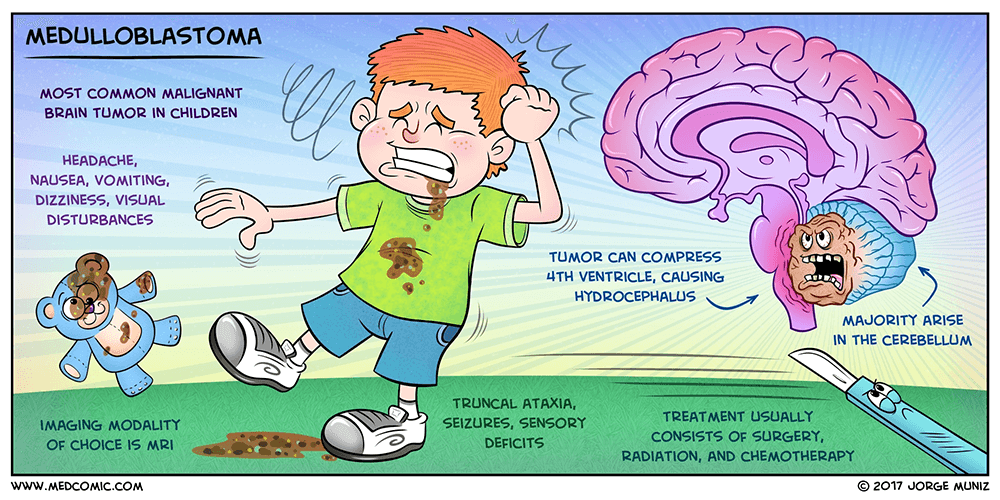
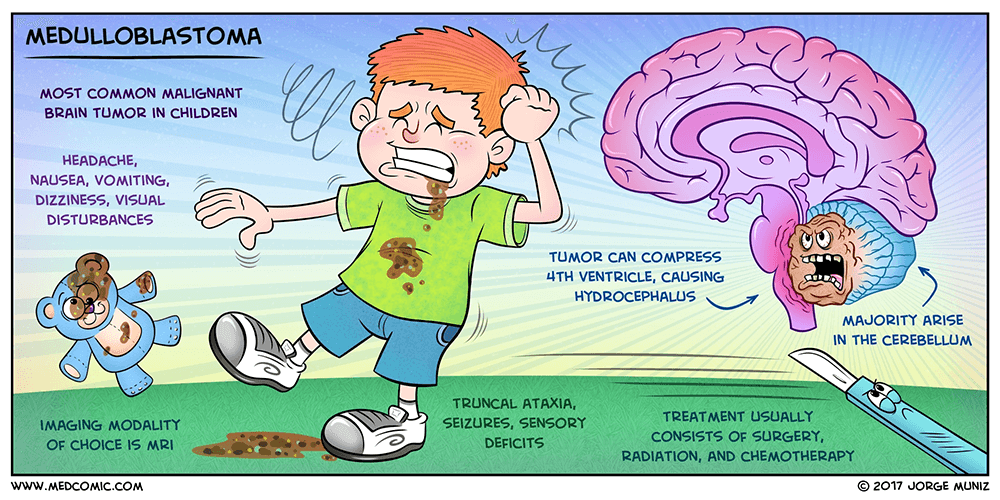
Medulloblastoma (MB) is an embryonic tumor of the neuroepithelial tissue and the most frequent primary pediatric solid malignancy. MB represents a heterogeneous group of cerebellar tumors characterized clinically by increased intracranial pressure and cerebellar dysfunction, with the most common presenting symptoms being headache, vomiting, and ataxia.
Epidemiology
MB is the most common malignant brain tumor in childhood. Annual incidence is estimated at 1/909,000 in Europe, 1.5/100,00 in the USA said Dr Prem Pillay , a Neurosurgeon who specializes in treating Medulloblastomas ( He trained at the Cleveland Clinic,USA and the Hospital for Sick Children, Toronto. Males are more affected than females.
Clinical description
Etiology
To date, the exact etiology of MB is still unknown but genomic data has identified multiple candidate genes that contribute to the pathogenesis of different subgroups of MB. This includes an inhibitor of the sonic hedgehog pathway SUFU (10q24.32), the RNA helicase DDX3X (Xp11.3-p11.23), chromatin regulators KDM6A (Xp11.2) and N-CoR complex genes BCOR (Xp11.4), and the Parkinson’s disease genes KMT2D (12q13.12), SMARCA4 (19p13.3), MYCN (2p24.3), and TP53 (17p13.1).
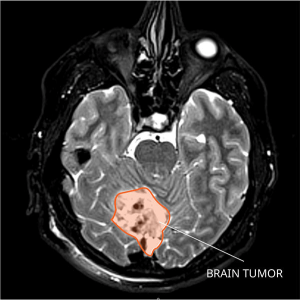
Diagnostic methods





Differential diagnosis
Differential diagnosis includes other brain tumors (ependymoma, glial tumor, atypical teratoid rhabdoid tumor; see these terms) and other causes of cerebellar alterations (infectious or cystic lesions, hemorrhages).
Management and treatment
Initially, patients need to be checked for increased intracranial pressure, which if present, needs to be controlled either by drugs (e.g. steroids) or by neurosurgical drainage (e.g. external drainage).
The best current treatment is gross total resection of the Tumor using Microsurgery assisted with Computer aided Image guided technology, Neuromonitoring particularly of brainstem signals followed by good ICU care stated Dr Prem Pillay who specializes in brain tumors including Medulloblastomas. The postoperative treatment depends on age, histological variant, and result of staging assessments. In children older than 3-5 years, combinations of chemotherapy and craniospinal irradiation including Stereotactic Radiotherapy with MicroMLC technology can be applied. In younger children, brain sparing therapies avoiding irradiation can be administered in very specific constellations.
Prognosis
The overall survival rates are now 80% in standard risk patients, and 30-60 % in high-risk patients.
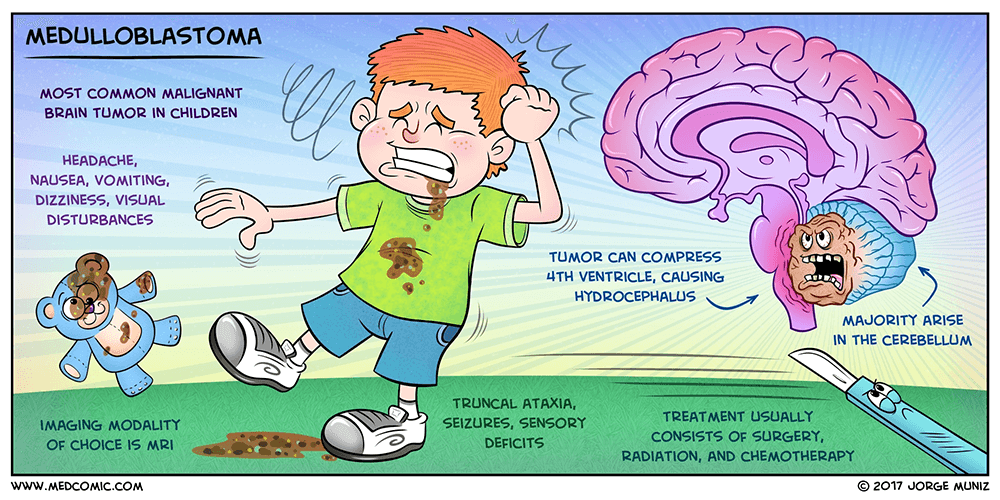
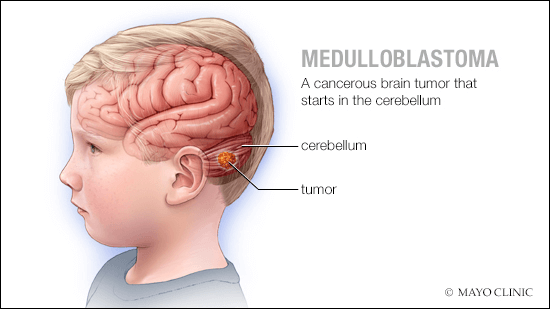
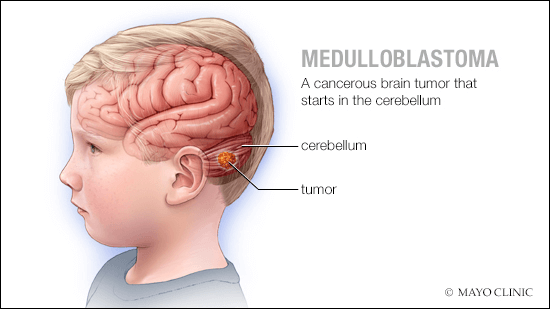
MEDULLOBLASTOMA
Definition
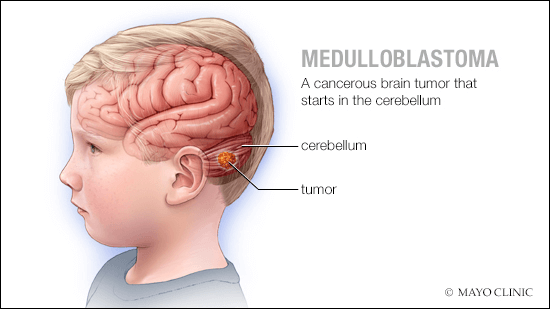
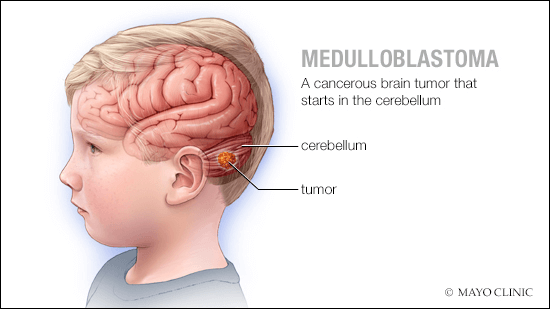
Medulloblastoma (MB) is an embryonic tumor of the neuroepithelial tissue and the most frequent primary pediatric solid malignancy. MB represents a heterogeneous group of cerebellar tumors characterized clinically by increased intracranial pressure and cerebellar dysfunction, with the most common presenting symptoms being headache, vomiting, and ataxia.
Epidemiology
MB is the most common malignant brain tumor in childhood. Annual incidence is estimated at 1/909,000 in Europe, 1.5/100,00 in the USA said Dr Prem Pillay , a Neurosurgeon who specializes in treating Medulloblastomas ( He trained at the Cleveland Clinic,USA and the Hospital for Sick Children, Toronto. Males are more affected than females.
Clinical description
Etiology
To date, the exact etiology of MB is still unknown but genomic data has identified multiple candidate genes that contribute to the pathogenesis of different subgroups of MB. This includes an inhibitor of the sonic hedgehog pathway SUFU (10q24.32), the RNA helicase DDX3X (Xp11.3-p11.23), chromatin regulators KDM6A (Xp11.2) and N-CoR complex genes BCOR (Xp11.4), and the Parkinson’s disease genes KMT2D (12q13.12), SMARCA4 (19p13.3), MYCN (2p24.3), and TP53 (17p13.1).
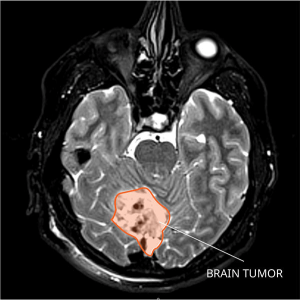
Diagnostic methods





Differential diagnosis
Differential diagnosis includes other brain tumors (ependymoma, glial tumor, atypical teratoid rhabdoid tumor; see these terms) and other causes of cerebellar alterations (infectious or cystic lesions, hemorrhages).
Management and treatment
Initially, patients need to be checked for increased intracranial pressure, which if present, needs to be controlled either by drugs (e.g. steroids) or by neurosurgical drainage (e.g. external drainage).
The best current treatment is gross total resection of the Tumor using Microsurgery assisted with Computer aided Image guided technology, Neuromonitoring particularly of brainstem signals followed by good ICU care stated Dr Prem Pillay who specializes in brain tumors including Medulloblastomas. The postoperative treatment depends on age, histological variant, and result of staging assessments. In children older than 3-5 years, combinations of chemotherapy and craniospinal irradiation including Stereotactic Radiotherapy with MicroMLC technology can be applied. In younger children, brain sparing therapies avoiding irradiation can be administered in very specific constellations.
Prognosis
The overall survival rates are now 80% in standard risk patients, and 30-60 % in high-risk patients.
