SYRINGOMYELIA:
A SERIOUS SPINE/SPINAL CORD DISEASE THAT NEEDS EARLY RECOGNITION AND TREATMENT
DR PREM PILLAY
SENIOR CONSULTANT NEUROSURGEON AND SYRINGOMYELIA EXPERT (INCLUDING COMPLEX SYRINGOMYELIA)
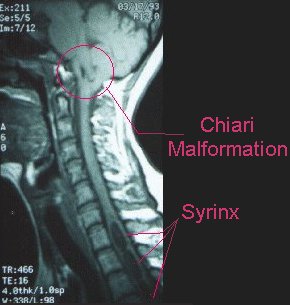 Syringomyelia is a chronic neurological disorder characterized by the formation of a fluid-filled cavity or cyst, known as a syrinx, within the spinal cord[1][3]. This condition can progressively expand over time, compressing or destroying surrounding nerve tissue and leading to a wide variety of symptoms depending on the size and location of the syrinx[1]; including muscle weakness, numbness, pain, headaches and bladder/bowel incontinence explains Dr Prem Pillay a Syringomyelia Expert and Neurosurgeon. If syringomyelia extends upwards to the brainstem its called Syringobulbia. Such patients have difficulty in swallowing, facial weakness, speech problems, giddiness and unsteady gait [20].
Syringomyelia is a chronic neurological disorder characterized by the formation of a fluid-filled cavity or cyst, known as a syrinx, within the spinal cord[1][3]. This condition can progressively expand over time, compressing or destroying surrounding nerve tissue and leading to a wide variety of symptoms depending on the size and location of the syrinx[1]; including muscle weakness, numbness, pain, headaches and bladder/bowel incontinence explains Dr Prem Pillay a Syringomyelia Expert and Neurosurgeon. If syringomyelia extends upwards to the brainstem its called Syringobulbia. Such patients have difficulty in swallowing, facial weakness, speech problems, giddiness and unsteady gait [20].
Definition and Overview
Syringomyelia occurs when cerebrospinal fluid (CSF), which normally flows around the outside of the brain and spinal cord, collects inside the spinal cord itself[4]. The resulting cyst can grow larger over time, potentially causing damage to the spinal cord and leading to pain, weakness, and stiffness[4]. This condition is most common in adults between the ages of 20 and 40, with men being more susceptible than women[3].
The terminology used to describe syringomyelia can be complex. It may also be referred to as hydromyelia, syringohydromyelia, or Morvan disease[3]. Some cases are classified as congenital (or communicating) syringomyelia, while others are considered acquired (or primary spinal/noncommunicating) syringomyelia[3].
Causes Of Syringomyelia
The exact mechanisms behind syringomyelia development are not fully understood. However, several factors have been identified as potential causes:
- Chiari Malformation: The majority of syringomyelia cases are associated with Chiari malformation, particularly Type I[1][3][20]. This congenital condition causes the lower part of the brain to protrude into the spinal canal, disrupting normal CSF flow[3][4][20][21].
- Spinal Cord Injury (SCI): Trauma to the spinal cord such as a sports injury or vehicular injury can lead to syringomyelia, sometimes months or years after the initial injury[3][4][20].
- Spinal Cord Tumors: Tumors such as astrocytomas, ependymomas, spinal cord metastases and other spine tumors can interfere with the normal flow of CSF, potentially leading to syrinx formation[4][20].
- Meningitis with or without Encephalitis: Inflammation of the membranes surrounding the brain and spinal cord can contribute to syringomyelia development[4].
- Tethered Spinal Cord: This congenital condition or acquired syndrome, where tissue attachments such as a short and thick filum terminale can limit spinal cord movement, and can cause syringomyelia[4][20][22].
- Idiopathic Cases: In some instances, no clear cause can be identified[3].
Symptoms of Syringomyelia of the Spinal Cord
Syringomyelia symptoms typically develop slowly over time, although they can appear suddenly after an accident[3]. Symptoms depend on the location and extent of the syringomyelia. Some patients may only have cervical spinal cord (neck) syringomyelia and have predominantly upper body and arms/hands symptoms. Common symptoms include:
– Pain in the neck, shoulders, arms, and hands
– Muscle weakness and wasting, particularly in the hands, arms, and shoulders
– Numbness or decreased sensation, especially to hot and cold
– Stiffness in the back, shoulders, arms, and legs
– Uncoordinated movements (ataxia)
– Scoliosis (abnormal curvature of the spine)
– Changes in bowel and bladder function
– Headaches
– Horner syndrome (in cases where the cyst affects nerves controlling eye muscles)[3][20]
Diagnosis of Spinal Cord Syringomyelia
Diagnosis of syringomyelia typically involves the following steps:
- Medical History and Physical Examination: The Neurosurgeon will review the patient’s symptoms and medical history, and perform a thorough neurological examination[4][20].
- Magnetic Resonance Imaging (MRI): This is the primary diagnostic tool for syringomyelia. MRI can provide detailed images of the spinal cord and any syrinx present[4]. MRI may also be done of the brain to look for Chiari Malformations, and also syringomyelia affecting the brainstem (syringobulbia)[20].
- Computed Tomography (CT) Scan: While less commonly used, CT scans may be employed in some cases[4][20].
- Electromyography (EMG)/Nerve Conduction tests (NCS): This test can help assess muscle and nerve function[4][20].
In some cases, syringomyelia may be discovered incidentally during tests ordered for other medical reasons[5].
Treatment of Spinal Cord Syringomyelia
The treatment approach for syringomyelia depends on the severity of symptoms and the underlying cause. Options include:
- Monitoring: For mild cases without significant symptoms, regular monitoring through MRI scans and neurological examinations may be sufficient[5][20].
- Surgery/ Microsurgery: Surgery/ Microsurgery: When symptoms are severe or progressive, surgical intervention is often necessary. The main goals of surgery are to relieve pressure on the spinal cord and restore normal CSF flow[4][5][20]. Surgical options include:
- Chiari Decompression: For cases associated with Chiari malformation, this surgery involves removing a small portion of the skull with or without a duropolasty ; creating more space for the cerebellum and tonsils to reduce pressure and improve CSF flow[5][20].
- Syrinx Drainage: A shunt may be inserted to drain fluid from the syrinx[5]. These shunts include syringo-arachnoid (SA) shunts and syringo-peritoneal (SP) shunts. This reduces the syrinx pressure on the spinal cord so that nerve recovery may occur.
- Obstruction Removal: Surgical removal of tumors or bone protrusions that obstruct CSF flow[5].
- Correction of Spinal Abnormalities : Procedures to address issues like tethered spinal cord[5]. Microsurgical release of the tethered cord may also relieve the syringomyelia.
- Pain Management: Medications may be prescribed to manage pain associated with syringomyelia[4].
- Physical Therapy: This can help maintain muscle strength and function [4].
Latest Innovations and Research
Recent advancements in syringomyelia research and treatment include:
- Stem Cell Therapy: A case study reported successful treatment of syringomyelia using uncultured umbilical cord-derived mesenchymal stem cells (UC-MSCs). This approach showed promise in alleviating pain and potentially reducing syrinx size[2]. However this type of treatment is still experimental and needs more clinical work to know whether it will be useful in the future.
- Natural History Study: The National Institute of Neurological Disorders and Stroke (NINDS) is conducting a five-year study to better understand the factors influencing syringomyelia development, progression, and treatment response[6].
- Cell Damage Reversal: NIH-funded scientists are exploring ways to stop and reverse cell damage caused by spinal cord injuries, which could have implications for syringomyelia treatment[6].
- Advanced Imaging Techniques: Ongoing research aims to improve diagnostic accuracy and treatment planning through enhanced MRI protocols and other imaging modalities[12][20].
- Postural Stability Research: Studies are being conducted to quantify postural stability in pediatric patients with Chiari malformation, which is closely associated with syringomyelia[12][21].
In conclusion, syringomyelia remains a complex neurological disorder with varied presentations and causes. While microsurgical interventions are currently the primary treatment for severe cases, ongoing research into stem cell therapies, advanced imaging techniques, and the natural history of the disease offers hope for improved diagnostic and therapeutic approaches in the future. As our understanding of the condition grows, so too does the potential for more effective and less invasive treatments for those affected by syringomyelia.
With many years of experience in treating syringomyelia including complex forms and access to the latest technological advancements, Dr Prem Pillay endeavours to offer patients the highest standard of care. From accurate diagnosis to tailored treatment plans, our approach aims for the best possible outcomes for individuals affected by this challenging condition.
If you or a loved one has been diagnosed with Syringomyelia, we welcome you to seek consultation with our specialized team. Together, we can develop a comprehensive evidence based and personalized treatment strategy that addresses your unique needs and provides the best chance for a positive outcome.
